Even in utero, babies do EXACTLY what they want to do…So what do you do if you are about full-term and the baby isn’t in the right position; i.e., BREECH?!!!
Pump your brakes, slow down Sally, don’t avail yourself of a c-section JUST yet…
Aside from options ranging from manipulation from Chiropractors that are supposed to make the baby flip, to certain “exercises” that are supposed to coerce the baby into assuming the correct position; i.e., vertex or head down (I’m still not convinced that any of the aforementioned actually work but hey, I’m open to it…).
Factors That Could Cause a Breech Presentation
Before we talk about what you need to know about External Cephalic Version, let’s discuss factors that may contribute to a fetus being in breech presentation. They include but are not limited to the following:
- Too much or too little fluid around the fetus (technically known as polyhydramnios and oligohydramnios respectively)
- The uterus is not normal in shape or has growths such as fibroids
- The fetus is preterm.
Occasionally, fetuses with certain birth defects will not turn into a head-down presentation prior to delivery. Breech presentations occur in 3-4% of full-term pregnancies.
What is External Cephalic Version?
Ok, now that we’ve discussed possible reasons for the breech presentation, let’s talk external cephalic version.
Like a Version… Touched for the very first time (In my BEST Madonna voice…..Gotta love Madge)
Speaking of touching… versions are typically performed by your OB/GYN. They are performed in a hospital setting.
External cephalic versions or just versions are performed when fetuses are in a non-vertex presentation.
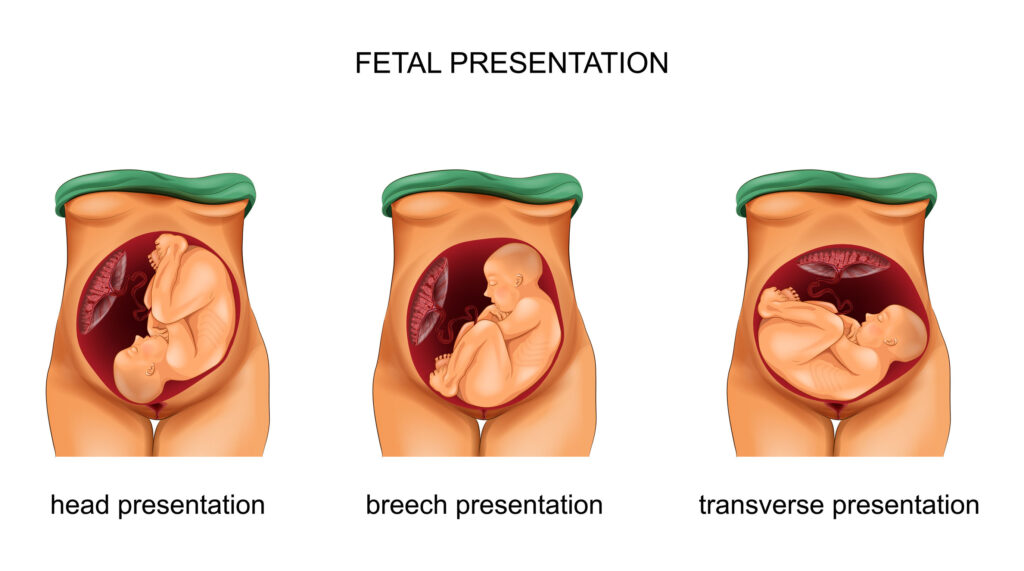
What is a non-vertex presentation?
When the fetus is presenting any way other than head down; that is, the fetus may be transverse (side-lying), or in a breech position (either the feet or buttocks are the presenting parts in the pelvis).
External Cephalic Version Procedure
The procedure itself involves your ob-gyn placing both hands on your gravid/pregnant uterus; one hand on the fetus’ head, the other near the buttocks, and attempting to roll/push the baby so that it flips into a head-down position.
Depending on how the fetus is lying, the roll may be either forward or backward. You may or may not experience discomfort during a version attempt. This depends on whether or not your uterus starts to contract due to the version attempt and the amount of pressure your doctor is using to flip the fetus.
If the first version attempt is not successful, there may be another attempt. If your uterus is contracting, you may be given medication to help relax your uterus. The most common medication given in this situation is Terbutaline.
You may also, alternatively, be given an epidural which serves two purposes. One, to relax the uterus, and two, to help with any ensuing discomfort.

Find out what the protocol is for versions at your particular institution. Please note that versions are performed in a hospital, typically on labor and delivery where immediate access to an operating room is available in case an emergency c-section is needed.
Is anesthesia involved? Some folks utilize it, others don’t (note the previously mentioned epidural above).
There typically will be some sort of fetal monitoring beforehand, to ensure that baby’s status is reassuring, and afterward, to ensure that baby is doing ok.
This involves the use of external monitors on the abdomen to monitor uterine activity (looking for the presence of contractions), and fetal heart rate to ensure fetal well-being.
After all, if you had just been flipped around in your dwelling place wouldn’t you want us to make sure you were doing ok; that is, no obvious signs of distress, labor, bleeding, etc?
There should be a bedside ultrasound that will monitor the baby throughout the procedure to ensure that the baby is moving in the right direction and that the heart rate remains stable………What sort of flip are we doing here anyway? Front or back? These are ALL things you need to know.
If you are RH negative; you will likely, or should, receive a dose of RhoGam. Versions, after all, can be a bit traumatic, especially when you consider that we are turning the baby inside the uterus.
What makes you a good candidate for a version?
- Being multiparous (that is, this isn’t your first baby)
- Having an adequate amount of amniotic fluid
- The baby is not engaged in the pelvis
What makes you a poor candidate for a version?
- This is NOT a singleton pregnancy…Versions should be done on single intrauterine pregnancies
- Low Amniotic Fluid Level
- Placental abnormalities, whether it be placental insufficiency, Previa, abruption, etc.
- Any uterine malformation or fetal anomaly
While being obese certainly is not a contraindication, it certainly may make the version technically more difficult. The size of the baby, location of the placenta, as well as location of the fetal back are other factors that impact success.
When is an External Cephalic Version Done?
Most versions are done at the 37-week mark. They are typically not performed prior to this due to the increased success rate noted at 37 weeks, as well as avoidance of preterm delivery if complications arise.
If successful, there is a 3% chance of reversion. Success rates have been quoted anywhere from just over 50% to around 63%. It’s probably worth asking your clinician what their success rate is.
External Cephalic Version Risks
While the whole purpose of an external cephalic version is to avoid a c-section, risks associated with it include things like: the fetus reverting to breech presentation, ensuing labor, premature rupture of membranes, fetal distress/bleeding, or any other “thing” that might necessitate an emergency delivery.
For those of you not comfortable with taking the risks associated with an attempted version, a c-section for malpresentation can always be scheduled at 39 weeks. Just make sure that you review the pros and cons so that you can make an informed decision.
Hoping this blog post adds value to your day!
Until Next Time,
Choose happiness.
Dr. Angela