How could I NOT do a blog post on cervical cancer? I mean, as an ob-gyn, I am THE QUEEN of one of THE MOST effective cancer screening tests; the pap smear. Cervical cancer is strongly associated with the human papillomavirus, more commonly known as HPV.
Before your heads start spinning out of control and you start getting nervous and anxious like most do when they visit their friendly gynecologist, let’s take our time and get through this. We’ll talk about pap smears, who, what, when, where, and why.
We’ll discuss HPV, who gets it, and the sequelae associated with it. We will discuss one of the BIG C’s, cervical cancer, its signs, symptoms, and what the next steps are once given the diagnosis.
Any questions? Let’s go.
Pap smears, the screening test for cervical cancer, start at the age of 21. The actual test itself has never been one of the top 3 favorite things women like to have done. It’s like who would you rather? The dentist or the gynecologist?
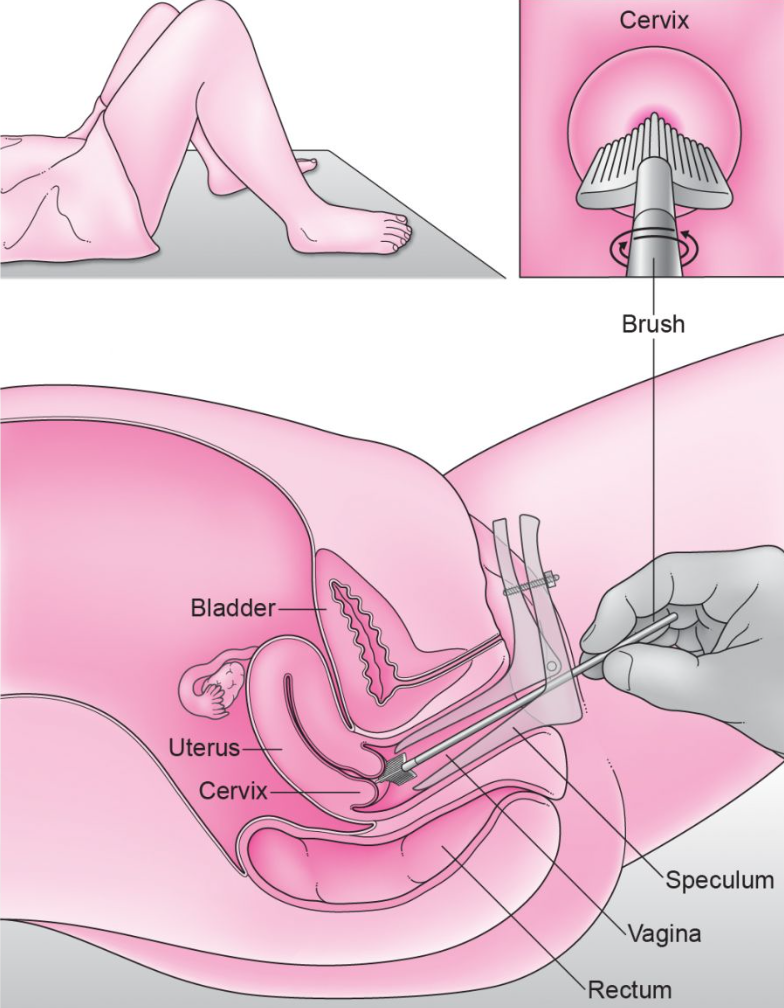
A pap smear is performed by visualizing the cervix, which is at the top of the vagina. This visualization is obtained by inserting and opening a speculum inside the vagina. Speculums are not one size fits all, so no worries, we will find one that suits your vagina just fine.
The cervix looks like a doughnut; i.e., a circle with a hole in it. The cervix represents the lower aspect of the uterus. A cytobrush, spatula, cervical broom, or any combination of the aforementioned are used to obtain a sampling of cells from the inside and surface of the cervix. These cells are in turn sent to the lab for evaluation.
In persons age 21-29, HPV testing is not typically performed. In this age group, HPV testing is done reflexly; i.e., if there is an abnormality found on the pap smear. In women aged 30-65, HPV co-testing, i.e., testing for HPV at the time the pap smear is performed.
How often you get pap smears is a conversation that should be had between you and your ob-gyn. In women under 30, as long as there are no previous abnormalities, a pap smear can be done every 3 years. In women between the ages of 30 and 65, either a pap with no HPV testing can be done every three years, or a pap smear with HPV co-testing can be done every 5 years.
Having said this, regardless of how often you decide to get your pap smear, you should see your obstetrician/gynecologist annually.
Remember, the pap smear is but a small part of your annual exam. The remainder of your exam allows a review of your medical history, assessment for risk factors for other medical issues, an ascertainment of your current health/fitness, a breast exam, an opportunity to discuss any transitional phases in your life that may be up and coming. Things like family planning, peri-menopause, menopause, come to mind.
Pap smears do not need to be done annually; here’s why. The one thing we’ve learned is that cervical cancer does not develop overnight. It’s a process; hence, it’s ok to not overscreen

HPV. We can’t talk about cervical cancer, and pap smears without mentioning HPV. Human papillomavirus is a sexually transmitted infection. It is very common.
In fact, 80% of the population has been infected with HPV at some point in their lifetime. To make the life of a gynecologist easier, we divide HPV into two groups; low risk, and high risk.
Low-risk HPV types are associated with things such as genital warts. High-risk HPV types, specifically type 16, 18, and 45 are associated with cervical cancer. In most, HPV is a virus that can be cleared on its own. Specifically, in healthy individuals, most HPV infections are asymptomatic and will resolve without issue.
HPV can be associated with cancers of the vulva, vagina, penis, anus, mouth, and throat. Safe sex practices are highly encouraged. Barrier contraception, as well as having an open conversation with new partners about their sexual history, practices, etc, will help decrease acquisition and passage.
As pertains to pap smears, HPV can cause transient cervical abnormalities such as low-grade lesions. These typically resolve on their own and require little more than observation. Other, high-risk forms of HPV, can be associated with more significant lesions such as high-grade abnormalities. These have a higher propensity of developing into cervical cancer and hence require more aggressive management.
Pap smear abnormalities are typically confirmed through an in-office procedure called a colposcopy. A colposcopy is an opportunity for your gynecologist to look at your cervix under high magnification.
The set up for a colposcopy is just like a pap smear in that a speculum is inserted into the vagina to allow adequate visualization of the cervix. The cervix is then painted with a vinegar-like solution to help highlight any areas of concern. Based on the appearance of the cervix, biopsies may or may not be performed.
The purpose of colposcopy is to confirm pap smear findings and to ensure that there isn’t a more significant abnormality present.
In addition to safe sex practices, the HPV vaccine is an effective way to protect against the types of hpv that have the highest association with cervical cancer. The HPV vaccine is most effective when administered to girls and boys age 11-12, is typically given through age 26, but can be given after age 26 in those individuals that have never been vaccinated and are at risk for HPV infection.

Pap smears. HPV. Cervical Cancer. Pap smears screen for cervical cancer and we’ve addressed that certain types of HPV have a strong association with cervical cancer. Cervical cancer occurs when the cells that typically make up the cervix become abnormal. This abnormality typically manifests as cells dividing much more rapidly than usual, invading deeper tissue layers, and eventually either spreading to other organs or forming a mass/tumor.
It typically takes several years for cervical cancer to develop which is why screening tests such as pap smears that can detect early cell changes are important.
Risk factors for cervical cancer include; early age of first intercourse (earlier than 18 years of age), having multiple sexual partners, having sexual partners with a high-risk profile (high risk as defined by types of sexual activity, and/or the number of sexual partners).
Other risk factors include smoking, personal history of vulvar, cervical, or vaginal dysplasia, family history of cervical cancer, and a history of sexually transmitted infections.
Remember, HPV is an STI (sexually transmitted infection), and where there is one, there are bound to be others; i.e., chlamydia, gonorrhea, the list goes on and on.
Initial signs of cervical cancer can include things like abnormal bleeding, spotting, or watery discharge from the vagina. Bleeding or spotting may occur after sex. Pelvic pain, issues with urination, swelling of the lower extremities can be signs of advanced disease.
Once cervical cancer is diagnosed, it is confirmed via colposcopy as previously discussed. The colposcopy will provide a biopsy for confirmatory purposes. Once confirmed, cervical cancer will need to be staged to determine extent of invasion and spread to neighboring organs.
This can be accomplished through various procedures such as a thorough pelvic exam, a colonoscopy, and cystoscopy to evaluate the bladder and bowel respectively. Imaging techniques may also be utilized to assess lymph node involvement.
As a generalist, once a diagnosis of cervical cancer has been established, I refer to a specialist for further management and treatment. That specialist is a gynecologic oncologist. Treatment options for cervical cancer range from hysterectomy to radiation therapy to chemotherapy depending on the stage of your cervical cancer.
Cervical cancer, one of the big C’s that can affect women, while scary, is preventable. Please, make yourself a priority and stay up to date with your screening.