Ovarian cysts account for emergent visits to the emergency department and subsequent follow-up with Ob-Gyns.
Why? Because they are a common cause for pelvic pain significant enough to stop you in your footsteps, cause you to double over in pain, and become completely incapacitated.
The usual presentation is “I was going through my normal day-to-day activities when all of a sudden, out of nowhere, I got this pain that was so bad I couldn’t move.” Or, “I got this sudden pain that woke me out of a dead sleep.”
Sound familiar?
I see a lot of women in the office with ovarian cysts. The usual recommendation from the emergency room is to follow up with your Ob-Gyn.
The usual workup is pretty simple. Most of the time they will, of course, order a pregnancy test, do some blood work, check your urine, and as far as imaging goes, they usually order a CT scan.
A CT scan is a good way not only to image your ovaries but also to rule out appendicitis. In other words, to make sure your appendix isn’t inflamed or hasn’t ruptured.
Because I see this so often, and because all women get them. Let’s talk about ovarian cysts.
Depending on where you are in your menstrual cycle, you will, at some point, develop ovarian cysts. Most of the time, they come and resolve on their own.
They only become a problem when they persist, become too large, twist on themselves (this is referred to as torsion), or burst (rupture). A ruptured ovarian cyst is painful enough that I’ve admitted women to the hospital to manage the pain.
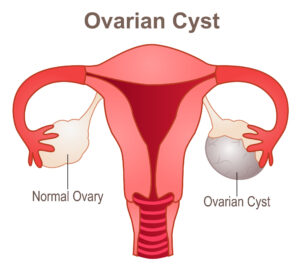
What is an Ovarian Cyst?
An ovarian cyst is a sac that forms either in or on the surface of the ovary. The sac can be filled with various substances, but the most common are fluid or/or blood.
Women have two ovaries; one on each side of the uterus. The ovaries are about the size and shape of a walnut. The ovaries are responsible for the development and release of eggs or ova each month during a woman’s menstrual cycle.
If the ova/egg is fertilized by a sperm, a pregnancy ensues thereafter. If the egg released by the ovary is not fertilized, it is shed monthly as a woman’s period or menstrual cycle.
Types of Ovarian Cysts
There are numerous types of ovarian cysts, they include:
Functional Cysts
Remember I mentioned all women getting ovarian cysts depending on where they were/are in their menstrual cycle? Well, these are functional cysts.
Every month your ovaries grow cyst-like structures called follicles. Follicles produce progesterone and estrogen and are responsible for releasing an egg when you ovulate. If a follicle continues to grow it is known as a functional cyst.
There are two types of functional cysts:
- Follicular cysts: Around midway through your menstrual cycle an egg bursts out of its follicle and travels down the fallopian tube (this is commonly referred to as ovulation). A follicular cyst forms when the follicle doesn’t release its egg but continues to grow.
- Corpus Luteum cyst: Once a follicle ruptures and releases its egg (ovulation), it begins producing estrogen and progesterone for conception. The follicle is now known as a corpus luteum cyst. There are occasions when fluid can accumulate inside the follicle causing the corpus luteum to develop into a cyst.
Functional cysts are commonly referred to as physiologic cysts. They are typically harmless, rarely cause pain, and usually disappear on their own within 2-3 menstrual cycles.
Other cysts that I commonly encounter that are not related to the normal function of your menstrual cycle include:
Dermoid cysts
Dermoid cysts are one of the more “eyebrow-raising” cysts I encounter. They can contain hair, teeth, cartilage, and tissue because they arise from embryonic cells.
Dermoid cysts are also known as teratomas. They are rarely cancerous but can become large (anything greater than 5 cm is considered large). So much so that they can cause the ovary to become displaced.
This in turn increases the ovaries’ risk of twisting on itself; this is called ovarian torsion. Ovarian torsion can cause significant pain as well as an acute onset of nausea and vomiting.
An ovary twisting on itself can result in either decreasing or stopping the flow of blood to the ovary. Ovarian torsion is a surgical emergency.
Cystadenomas
These cysts develop on the surface of the ovary and can either be filled with a mucinous or watery material. Cystadenomas can grow to pretty significant sizes. I have seen cystadenomas greater than 20cm in size.
Endometriomas
These cysts are a hallmark finding with endometriosis, the syndrome where cells that are normally shed as your menstrual cycle are shot out of the fallopian tubes and implant on various aspects of your abdomen and pelvis (visit our previous blog post on endometriosis).
These cells can implant on your ovary or ovaries and form endometriomas. They are also known as chocolate cysts.
Symptoms of Ovarian Cysts

Most ovarian cysts are completely asymptomatic (showing no symptoms). However, if they grow large, or rupture, they can cause significant symptoms such as:
- Pelvic pain. This will oftentimes be described as sharp or dull, in the lower abdomen, on the side of the cyst. Pain with sex is a common presenting symptom.
- Pressure. Patients will often describe a fullness or heaviness in their lower abdomen or pelvis. Constant pressure on the bladder is another common symptom.
- Bloating. This is when your belly feels swollen.
Risk Factors for Ovarian Cysts
Risk factors include:
Previous history of ovarian cysts. History is very telling. If you have had an ovarian cyst before, you are likely to have another one.
Endometriosis. As previously mentioned, endometriosis causes cells that normally line the inside of the uterus and are shed as a period every month to be shot out of the fallopian tubes and implant on various aspects of the abdomen and pelvis. The ovaries are no exception.
While endometriomas are commonly seen with endometriosis, you can have endometriosis without the presence of an endometrioma.
Of note, endometriomas have a classic appearance on ultrasound and are one of the sole ways to diagnose endometriosis on imaging as you can have a completely normal ultrasound and have endometriosis.
Hormones. Taking medications such as ovulation-inducing medications like Clomid increases your risk of ovarian cyst formation.
Severe pelvic infection. If the infection involves the ovaries, a cyst can form.
Ovarian cysts Complications
As previously stated, most ovarian cysts are harmless and resolve on their own. If there are to be complications, the most common ones include:
- Ovarian Rupture. If an ovarian cyst persists and grows to be a certain size, it is at an increased risk of rupturing. A cyst that ruptures can cause severe pain and/or bleeding. Sex or any other vigorous activity that involves the pelvis increases the risk of rupture.
- Ovarian Torsion. As previously noted, the larger an ovarian cyst is, the greater the risk of ovarian torsion. This is caused when the ovary is displaced due to the size of the cyst. This, in turn, causes the ovary to twist on itself. Common symptoms associated with torsion include severe pelvic pain, nausea, and vomiting.
- Cancer. This is certainly not encountered very often, but it’s a very real and serious complication. An ovarian malignancy may be found either on incidental imaging (such as a CT scan or an ultrasound) or routine pelvic examination. This is why it remains important to have regular Ob-Gyn visits.
Ovarian Cysts Diagnosis
A careful history and physical examination are the major ways to diagnose ovarian cysts.

As mentioned above, cysts can cause characteristic symptoms. If they get to be a certain size, they can also be felt on a pelvic exam.
Even if the cyst can’t be felt on examination, pain is a symptom that may or may not be suggestive of an ovarian cyst. Based on the history and physical, these findings will often lead to further diagnostic testing such as imaging tests.
CT (Computerized Tomography) Scan
As previously observed, ovarian cysts are a common reason women present to the emergency department. In the emergency department, the most common imaging study ordered for pelvic or lower abdominal pain is a CT scan.
This allows “killing two birds with one stone” so to speak. Specifically, a CT scan allows one to rule out either inflammation or rupture of the appendix, as well as to see if an ovarian cyst is present.
Ultrasound
The ultrasound is the gold standard of imaging in the realm of obstetrics and gynecology.
The common recommendation for follow-up from a trip to the emergency room when an ovarian cyst has been diagnosed is, “follow up with your GYN.” If only they would order an ultrasound before discharge.
The ultrasound gives the best imaging of the uterus and ovaries. It gives important details of the cyst, specifically size.
It also shows whether it is simple or complex, meaning, is the cyst filled with fluid, or blood, or does it have characteristic findings such as solid components, septations, thickened walls, papillary excrescences, etc.(the aforementioned are examples of findings that would make a cyst “complex”).
An ultrasound can also determine if blood flow is present in the cyst.
Laparoscopy
Laparoscopy is a minimally invasive surgical procedure that allows direct visualization of the uterus and ovaries. It is done under general anesthesia and is typically an outpatient procedure.
CA-125 blood test
If malignancy (cancer) is suspected, your physician may order this blood test, if the ovarian cyst has any of the features considered complex (see above) that would increase the risk of malignancy.
Of note, this blood test is very non-specific, in that many benign things can cause it to be elevated. Endometriosis, uterine fibroids, pelvic inflammatory disease are a few things that come to mind.
Treatment for Ovarian Cysts
To treat or not to treat, that is the question. Whether or not to treat will be based on the size of the ovarian cyst and symptoms.
Observation
If the cyst is small (less than 5cm), simple, and you are having no symptoms, the likely course of action is to do nothing

In most cases, your Ob-Gyn will order a repeat ultrasound in 2-3 months to document stability and/or resolution. The former is to ensure that the cyst has not increased in size, while the latter is to check if the cyst has resolved on its own.
Most small, simple cysts are asymptomatic and repeat imaging typically demonstrates that these cysts go away on their own.
Medication
For women with a history of recurring ovarian cysts, hormonal options, such as birth control pills, are very common. Most believe that birth control pills will prevent cysts from forming.
While I do believe that OCPS (oral contraceptive pills) decreases the risk of ovarian cysts forming, they do not totally eliminate their recurrence.
Surgery
The decision to proceed with the surgery is oftentimes dependent on presenting symptoms. If a woman is in significant pain that is interfering with her quality of life, she will be taken to surgery.
If she has an acute abdomen, sometimes referred to as a surgical abdomen, she will be taken to surgery urgently. If there is suspicion of ovarian torsion, surgery will be done more quickly. Depending on the size of the cyst, surgery may be recommended.
Remember, the larger the ovarian cyst size, the greater the risk of ovarian torsion and the greater the risk of ovarian rupture.
Most ovary cysts can be removed laparoscopically. Most ovarian cyst removal doesn’t require removal of the ovary. When only the cyst is removed, this is referred to as an ovarian cystectomy.
Depending on the characteristics of the ovarian cyst, your surgery may be referred to a gynecological oncologist.
Gyn-Oncologists specialize in cancers. If there is any suspicion that your ovarian cyst is malignant (cancerous), a Gyn-Oncologist will need to perform the surgery.
If there is a concern for malignancy, the surgery is much more involved than an ovarian cystectomy and would involve a total hysterectomy with removal of the uterus, ovaries, and fallopian tubes.
Staging would also be done at the time of the procedure. This involves pelvic washings, and lymph node dissection, and sampling. Oftentimes, depending on the stage of cancer, adjuvant therapy in the form of chemotherapy and radiation would need to be performed.
Conclusion
Because I deal with ovarian cysts all the time, and they are one of the most common reasons women either visit the emergency room or their Ob-Gyns, I thought it would be great to fill you in on a few of the more noteworthy details. It is my sincere hope that you gain some insight from this blog post.
Got questions? Leave them in the comments.
Until next time,
Choose happiness.
Dr. Angela.
FAQs
Natural remedies for ovarian cysts only help to manage and relieve symptoms. It doesn’t make the cysts disappear.
Cysts on the ovary are pretty harmless and not cause symptoms. However, ovarian cysts can rupture, and cause bleeding. Infected ovarian cysts that rupture can trigger sepsis – a life-threatening immune response to harmful bacteria.
You should get medical help if you’re experiencing sudden, severe abdominal pain. Abdominal pain with fever and vomiting. Faintness, dizziness, or weakness.
Dermoid cysts also called benign mature cystic teratomas are the only ovarian cysts that can run in families. 1 out of 10 dermoid cysts will develop in both ovaries.
Ovarian cysts and Polycystic Ovary Syndrome (PCOS) are related conditions, but they are different.
In PCOS, the ovaries have an abnormally large number of follicles on them, resulting in hormonal imbalance. Usually, women with PCOS will not develop cysts, but follicles.
Symptoms include:
- No period or irregular periods
- Weight gain
- Excessive body hair
- Thinning of head hair
- Inability getting pregnant
- Acne and/or oily skin
Ovarian cysts, on the other hand, are sac filled with fluids in or on the ovary. Most cysts occur as a result of menstrual cycles, and child-bearing years. They are pretty not dangerous and will go away on their own.
In some cases, cysts can be cancerous and increase the risk for ovarian cancer. Symptoms are similar to PCOS, except women with ovarian cysts don’t find it difficult to get pregnant. Ovarian cysts might also cause pelvic pain, lower back pain, bloating, and high blood pressure.