Endometriosis is the gynecological equivalent of preeclampsia as far as I’m concerned. In other words; I despise them both.
Seems I have been running a special on endometriosis of late. Literally, I have seen an influx of women with endometriosis. Management has been both medical and surgical.
I had a pretty impressive case a week or two ago where we removed two large endometriomas and ablated quite a bit of endometrial tissue/implants. The pre and post-surgery pictures were pretty impressive. I scored that particular case for team Dr. Angela.
Although there are small victories such as the one previously mentioned, endometriosis is an on-going battle. Who knows, the next round may not be so favorable for me.
Here are five things you need to know.
Top 5 Facts About Endometriosis
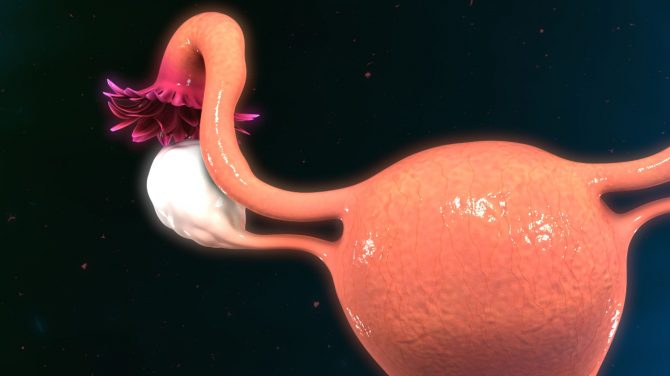
Endometriosis occurs when the cells that line the inside of the uterus, the endometrium, which is normally shed monthly as your menstrual period, gets shot out of the fallopian tubes and implants on various aspects of the pelvis; i.e., the tubes, ovaries, cul-de-sac, etc. Endometriosis can also implant on the bowels, appendix, scars….
The hallmark symptom of endometriosis is pelvic pain characterized by cyclical, painful, periods. The pain associated with endometriosis is oftentimes more severe than your typical period cramps. Endometriosis pain is often described as debilitating.

Other symptoms may include:
- Abdominal pain
- Pain during sex
- Bowel issues such as constipation/diarrhea (most commonly during your period)
Infertility - Painful bowel movements
- Pain with urination
- Pain associated with endometriosis may begin a few days prior to the onset of your menstrual period and/or extend several days into your menstrual cycle.
Causes of Endometriosis
No one knows for sure what causes endometriosis. There are, however, several theories. A few of the more popular ones are:
- Retrograde Menstruation: when menstrual blood containing endometrial tissue gets shot out of the fallopian tubes and implants on various aspects of the pelvis. These displaced endometrial cells in turn adhere to various aspects of the pelvis; be it other pelvic organs, pelvic walls, or as previously mentioned, other structures such as the bowel, appendix, etc. These cells, in response to hormones released by your ovaries, continue to grow, bleed and create an inflammatory response which can cause pain, and eventually scar tissue formation.
- Induction theory: peritoneal cells (cells that typically line the abdomen) are transformed into endometrial cells by hormones or immune factors.
- Endometrial cell transport: endometrial cells are transported to various aspects of the body via blood vessels.
- Surgical Scar Implantation: Endometrial cells attach to incisions made at the time of hysterectomy, c-section, etc.
Risk Factors
Although anyone can have endometriosis, some factors increase the likelihood of getting it.
- Family history is a BIG one; specifically, if you have one or more relatives (mother, aunt, or sister) with endometriosis.
- Short menstrual cycles; i.e., <28 days between periods. Early-onset periods, and heavy menstrual periods lasting longer than seven days.
- Alcohol consumption.
- Any medical condition that prevents the passage of menstrual blood flow out of the body; imperforate hymen and uterine anomalies come to mind.
Endometriosis typically develops several years after menarche (the onset of menstruation).
Diagnosis and Treatment
Diagnosing endometriosis involves a thorough history and exam.
Pay close attention to family history, social history, reproductive history such as the age of menarche, length, and heaviness of menstrual periods, and the signs/symptoms of endometriosis which we’ve already mentioned.
During the evaluation, a thorough pelvic exam will be done by feeling for large cysts (endometriomas), or scar tissue behind the uterus.
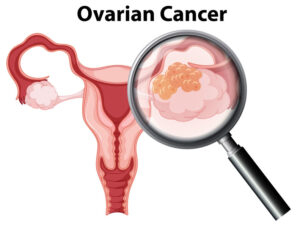
An ultrasound might reveal a characteristic finding such as an endometrioma, a cyst that is commonly associated with endometriosis. Endometriomas are also known as chocolate cysts. Other than an endometrioma, endometriosis doesn’t really have significant findings on ultrasound.
Endometriosis is more common than you think; don’t be so quick to write off the diagnosis.
Researchers believe that at least 11% or more than 6 and ½ million women in the United States between the ages of 15 and 44 are affected by endometriosis.
It is especially common in women in their 30s and 40s and may make it harder to get pregnant. Just an FYI, if a woman has primary infertility, i.e., trying to get pregnant with no history of previous pregnancies, endometriosis has to be on your radar.
Some clinicians may choose to diagnose and treat endometriosis based on symptomatology, others may choose to diagnose via a diagnostic laparoscopy, which is the gold standard.
Diagnostic laparoscopy can be performed if conservative measures fail. Conservative measures are medicinal; i.e., pain control, hormonal suppression, etc.
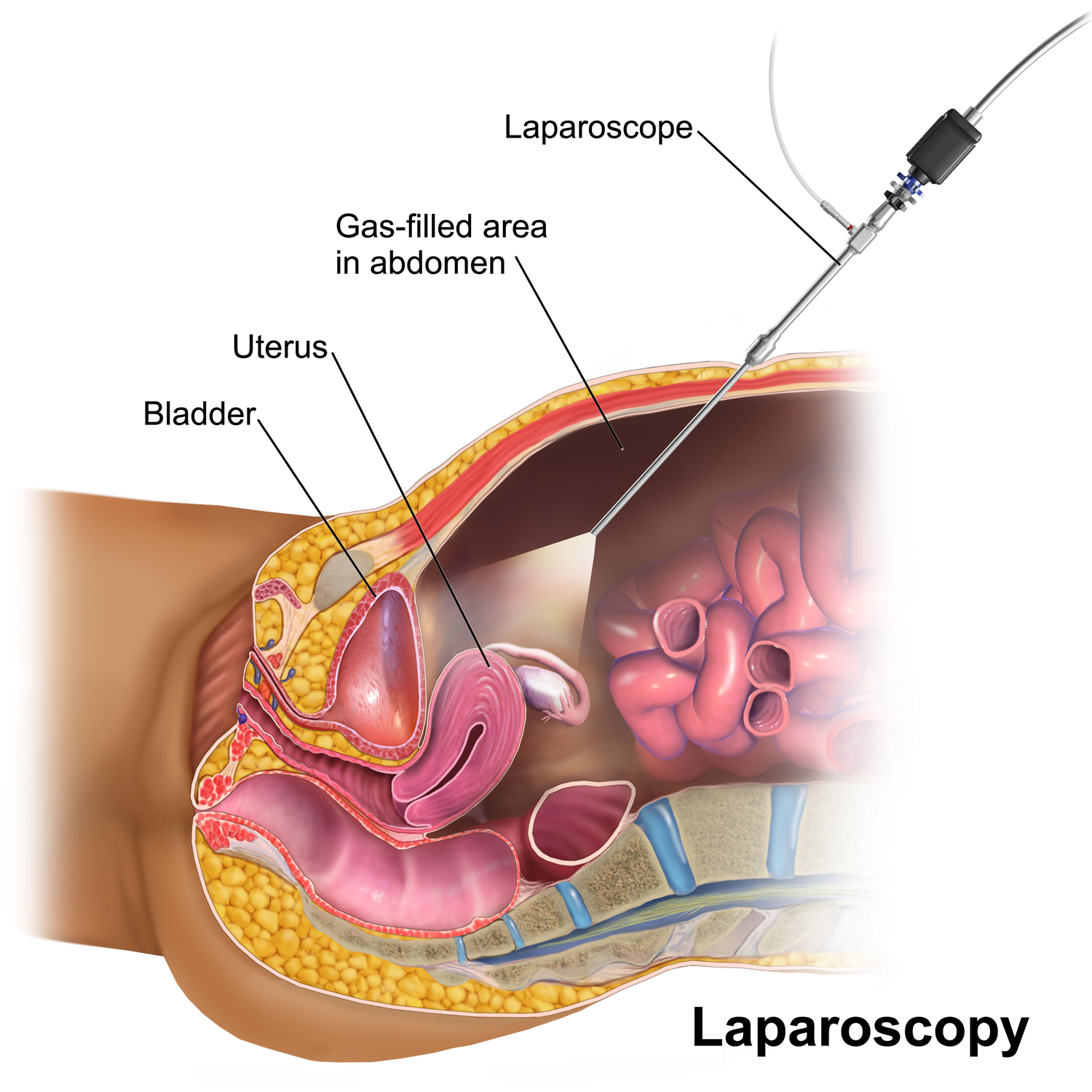
A laparoscopy is a minimally invasive surgery where the physician puts a camera through an incision in your belly button and thus is able to view the abdomen and pelvis in its entirety. If endometriosis is visualized, it can either be cauterized or excised. Cysts such as endometriomas can be removed.
Medical therapy includes medications aimed at treating pain. Non-steroidal medications such as Alleve, Ibuprofen, Motrin, and Naproxen are common examples.
Hormonal therapies (oral contraceptive pills, Depo-Provera, GnRH agonists, etc) aim to suppress hormonal fluctuations (largely responsible for endometrial growth, tissue breakdown, bleeding, and pain)associated with monthly menstrual cycles.
These are usually the first step in treatment for those not seeking to get pregnant.
Endometriosis can range from mild to debilitating. Symptomatic versus asymptomatic. Of note, the amount of endometriosis noted at the time of a laparoscopy does not necessarily equate to the amount of pain a woman may or may not experience.
Emotionally, it can take a HUGE toll on women; whether it’s the daily pain, or heartache that may be associated with infertility resulting from endometriosis.
Ultimately, the last-ditch option for treating endometriosis involves a complete hysterectomy with the removal of the ovaries and tubes.
Leaving the ovaries is typically not recommended, as the hormones produced by the ovaries can result in remaining endometrial tissue growing and causing pain.
It’s a wrap! Hoping this blog post has been informative. Would love to hear from you. If you happen to struggle with endometriosis, what has/hasn’t worked for you? I wanna know, leave your comments.
Until next time,
Choose Happiness.
Dr. Angela.