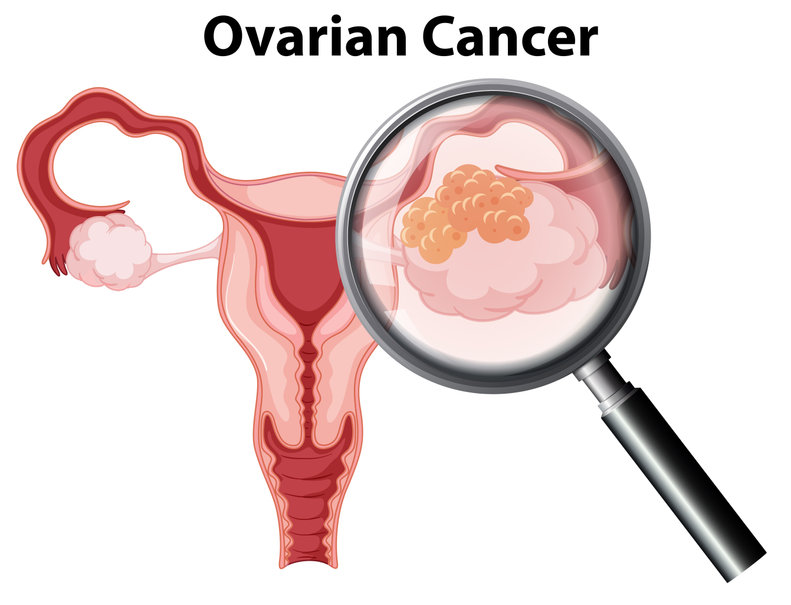
Types of Ovarian Cancer
The type of ovarian cancer depends on the type of cell in which cancer starts.
There are three types of cells in the ovary – epithelial cells, germ cells, and stromal cells.
- Epithelial ovarian cancer: cancerous tumors form in layers of the tissue outside the ovary. These types are the most common, with 90% of ovarian cancers being epithelial tumors.
- Germ cell ovarian cancer: cancerous tumors develop in the cells that produce eggs. This type is rare.
- Ovarian stromal tumor/cancer: cancerous tumors grow in the cells that produce hormones.
How to Detect Ovarian Cancer

Ovarian cancer is often referred to as “the silent killer.”
Why? Because by the time it is diagnosed, it’s usually in an advanced stage.
Pancreatic cancer is another malignancy with few signs/symptoms. Having said such, it is extremely important for women to report any signs or symptoms that may correspond to those previously mentioned.
Even if you are feeling just a bit “off,” don’t be afraid to see your friendly gynecologist. Remember, no one knows your body better than you do. Even if the work-up comes back showing nothing, at least you’ve taken the appropriate steps to ensure everything is ok.
While there are no screening tests for ovarian cancer, part of the workup will/should include a thorough history and exam.
History is important in an ovarian cancer workup to identify any risk factors that may put you at an increased risk of the diagnosis.
Risk factors can be broken down into two major categories: menstrual cycles (ovulation) and family history.
Age of menarche (when a woman starts her period) and menopause (when a woman stops having periods) is significant because the more a woman ovulates (has menstrual cycles) over her lifetime, the higher her risk of having ovarian cancer.
Thus, starting your period at a younger age, ending periods at a later age, and never getting pregnant, are important historical markers that put you at an increased risk of ovarian cancer.
Family history inquiries are needed to determine if you have sisters, mothers, or other relatives that have had or have ovarian cancer.
Up to 25% of ovarian cancers are related to family cancer syndromes. Because of this, all women with ovarian cancer should undergo testing for BRCA1 and BRCA2. If positive, family members of both sexes should be tested (siblings, children, etc).
The pelvic exam, while no one’s favorite exam, is a part of the workup. A pelvic exam is done to check for any irregularities such as masses.
Other tests that can be carried out include:
Blood tests. Multiple blood tests can be used to determine the likelihood of a woman having ovarian cancer. Let’s start with the CA-125. The CA-125 IS NOT a screening test. This test shouldn’t be drawn unless a mass is present.
In a postmenopausal woman, the presence of a pelvic mass and an elevated CA-125 is highly suggestive of cancer.
CA-125 is less accurate in younger women as there are numerous disease processes, including but not limited to, diverticulitis, irritable bowel syndrome, appendicitis, liver disease, stomach disease, etc, that can cause it to be falsely elevated.
Other blood tests such as OVA-1, ROMA are other blood tests used to help determine whether a pelvic mass will be cancerous.
Transvaginal Ultrasound (TVUS). This is the gold standard of imaging anything in the pelvis. This test uses sound waves to detect tumors in the ovaries and reproductive organs.
A mass on an ovary will have very characteristic findings that are suggestive of cancer including but not limited to: increased size, solid components, thickened walls, the presence of septations, etc.
Biopsy. This involves removing a small tissue from the ovary and examining it under a microscope. A laparoscopy might be used to remove the tissue.
Of note, by the time a patient goes to the OR (operating room), the physician, typically a gynecologist/oncologist, has a pretty good sense of the diagnosis based on lab work, imaging, e.t.c.
At the time of surgery, a sample of the tumor can be sent to pathology for a frozen section so that the appropriate surgery and staging can be performed.
Other imaging tests such as a CT scan or MRI scan can also be used.
Stages of Ovarian Cancer
There are 4 stages of ovarian cancer. Staging is the process used to classify a tumor based on the extent it has spread in the body at the time of diagnosis. Ovarian cancer is surgically staged.
Complete staging includes hysterectomy, removal of the ovaries, tubes, pelvic and aortic lymph node dissection, omental biopsies, and peritoneal biopsies. Staging determines treatment.
Stage 1
In Stage 1 ovarian cancer, the cancer is confined to one or both ovaries. It hasn’t spread anywhere.
Stage 2
In stage 2, cancer has spread to the uterus and other pelvic regions such as the fallopian tube or bladder (rectum).
Stage 3
In stage 3 ovarian cancer, cancer has spread beyond the pelvis to the lymph nodes and abdominal lining.
Stage 4
In stage 4 ovarian cancer, cancer has spread to distant areas of the body such as the lung or liver. This is the most critical stage of ovarian cancer.