Quick Facts about PCOS
- PCOS is a common hormonal disorder affecting women in their reproductive years.
- No one knows what causes PCOS. However, it has been linked to high androgen levels (the male hormone – testosterone).
- Symptoms usually include irregular periods, heavy bleeding, excessive hair growth, acne, overweight, presence of high levels of testosterone.
- To be diagnosed with PCOS, you should have 2 out of these 3. Irregular periods, cysts on the ovary, or high androgen levels.
- PCOS can be managed through modification of diet and lifestyle as well as other medical treatments.
Polycystic ovarian syndrome or P-Cose? I remember the first time a patient asked me to evaluate them for PCOS (P-Cose), I was like “what?!?!?” I had never referred to it like that.

In the realm of Ob-Gyn, we either refer to it as P-C-O-S or polycystic ovary syndrome. Nonetheless, once we finally got on the same page, the history and physical began.
I evaluate a lot of women for polycystic ovary syndrome, and the symptoms can vary. Some women feel as if their hormones are “off”. Others experience the inability to lose weight, irregular periods, increased hair, etc.
If you don’t have PCOS, you likely know someone who does. That’s how common it is among women.
Just what is PCOS? This blog post will attempt to address that and a whole lot more. Keep reading to find out.
What is PCOS?
While there is no universally accepted definition of PCOS, most would agree that it is a disorder characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries.
Let’s explain these terms in detail.
Hyperandrogenism
Androgens are secreted by the adrenal glands and ovaries. The ovaries secrete the male hormone – testosterone, in addition to the more commonly known estrogen and progesterone.
Signs of high androgen levels include increased acne (high testosterone levels can cause an increase in oil production which in turn can cause acne eruptions on the face, chest, back), and increased hair growth. Acne often leads to skin discoloration and dark spots, hence affecting the morale and confidence of the person. This drives many to resort to various skin-care products such as biopelle and alike, to gain back their lost self-esteem.
Due to PCOS, women will notice increased hair on the face, lower abdomen, chest, and back. Medically, this increased hair growth is called hirsutism.
I had a patient the other day that said that she shaved a few times a week to prevent having a full beard.
Ovulatory dysfunction
This presents as irregular periods. Irregular being defined as not occurring every month. Women with PCOS experience fewer than 8 periods a year to no periods at all.
Ovulatory dysfunction can also present as heavy bleeding.
With periods sometimes skipping up to months at a time, the uterine lining has the opportunity to build up more, and become thicker than usual. This results in a period that is heavier and/or longer than one might be used to.
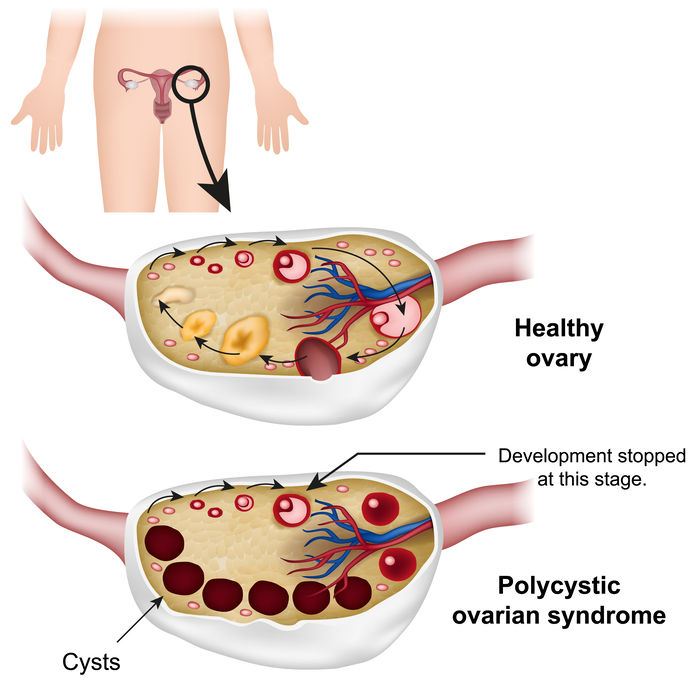
Polycystic ovaries
This is determined by ultrasound. ACOG defines polycystic ovaries, in one or both ovaries, as the presence of either 12 or more follicles between 2-9mm in diameter, or the presence of ovaries with increased volume(>10cm3).
Both ovaries don’t have to be polycystic in order to make the diagnosis.
Moving forward, PCOS is a hormonal issue affecting women during the childbearing years, and usually between the ages of 15-44. Up to 26.7% of women in this age group have PCOS.
PCOS affects a woman’s ovaries. If you will recall, the ovaries are responsible for producing estrogen and progesterone (the hormones that regulate the menstrual cycle), as well as testosterone.
Ovulation occurs when the ovaries release eggs. This usually occurs monthly.
Ovulation is controlled by FSH (Follicle-stimulating Hormone) and LH (Luteinizing Hormone). These hormones, produced by the pituitary gland, control ovulation.
FSH stimulates the ovary to produce a follicle (see previous blog post on ovarian cysts), a small sac/cyst-like structure that contains an egg. LH then causes the ovary to release the mature egg (ovulation).
PCOS is a “syndrome” in that it is a triad or group of symptoms affecting the ovaries and hence ovulation. As mentioned above, its three primary features are:
- Cysts on the ovaries
- High androgen levels
- Irregular periods as defined by either having few or no periods or very heavy periods.
By definition, “polycystic” means “many cysts.” As earlier said, one of the ultrasound findings in an individual with PCOS is the presence of 12 or more follicles surrounding the perimeter of the ovary.
These follicles contain immature eggs. The eggs never mature enough to trigger ovulation; hence the reason folks with PCOS have anovulatory cycles. Get it?
This lack of ovulation alters hormonal levels, that is, progesterone, estrogen, LH, FSH, and androgen levels. No wonder PCOS is characterized as causing a hormonal imbalance!
Causes of PCOS
If you have been wondering what causes polycystic ovary syndrome, the answer is no one knows for sure.
Most in the scientific community believe it is caused by high levels of androgens. This in turn prevents the normal production of hormones and hence egg production as we noted above.
Elevated androgen production has also been linked to genetics, insulin resistance, and inflammatory processes.
Genes
Studies reveal that PCOS runs in families. This is likely to be caused by more than one gene.
Insulin resistance
70% of women with PCOS have insulin resistance. This means that their bodies don’t adequately utilize the insulin.
The major symptom of insulin resistance is a skin condition known as acanthosis nigricans. Oftentimes seen in the groin, underneath breasts, or in the axilla (underneath arms in the armpit region), it is characterized by the skin having a dark, velvet-like appearance.
This is a common sign of insulin resistance and is commonly seen in persons with PCOS.
Of note, insulin is a hormone produced by the pancreas to help the body utilize sugar from foods for energy.
When our cells aren’t able to use insulin properly, our bodies are tricked into believing that it needs to produce more insulin; as a result, the pancreas produces even more insulin. Excess insulin causes the body to produce more androgens (male hormones).
Obesity is a major contributor to insulin resistance. Pair obesity and insulin resistance together and you have a recipe (increased risk) for type 2 diabetes.
Inflammation
Increased levels of inflammation are noted in the bodies of women with PCOS. Being overweight is thought to contribute to inflammation. Studies have linked elevated androgen levels to increased inflammation.
Are you noticing the role hyperandrogenism or excess androgen plays in the signs and symptoms associated with PCOS?
PCOS Symptoms
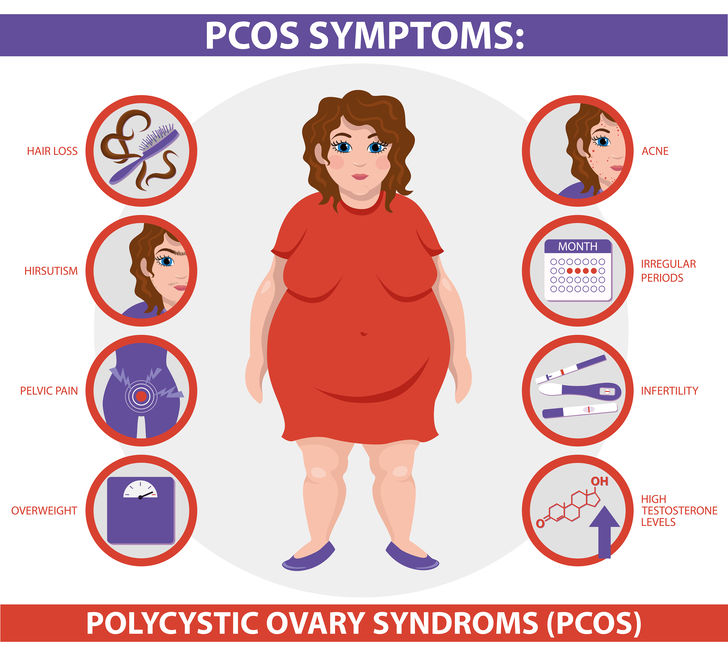
The most common symptoms associated with PCOS are:
- Irregular periods
- Heavy Bleeding
- Hair growth. Greater than 70% of women with this condition grow hair on their face and body Hirsutism is defined as excess hair growth.
- Darkening of the skin. (known as acanthosis nigricans).
- Headaches. Hormonal fluctuations can cause headaches in some women.
Effects of PCOS on Your Body
With the effects we’ve seen elevated androgen levels have on periods and ability to metabolize insulin, etc, does it come as any surprise that it also adversely affects fertility and other bodily functions?
Infertility
In order to get pregnant, you need to ovulate. Anovulation caused by PCOS is a common cause of infertility in women.
Metabolic Syndrome
80% of women with PCOS are either overweight or obese. Obesity and PCOS are risk factors for:
- High blood pressures
- High blood sugar levels
- Decreased HDL “good” cholesterol
- Increased LDL “bad” cholesterol
In accordance with ACOG, the above makes up metabolic syndrome which is diagnosed by the updated Adult Treatment Panel III criteria of:
- Elevated blood pressure (greater than or equal to 130/85),
- increased waist circumference (greater than or equal to 35 inches),
- elevated fasting glucose levels (greater than or equal to 100mg/dL),
- reduced HDL cholesterol levels (less than or equal to 50 mg/dL), and
- elevated triglyceride levels (greater than or equal to 150mg/dL)
Metabolic syndrome increases your risk for:
- Stroke
- Diabetes
- Heart Disease
Endometrial Cancer
Irregular periods and going months without shedding the lining of the uterus lead to a thickened endometrial or uterine lining. This is a risk factor and thus increases the risk for endometrial or uterine cancer.
Diagnosing PCOS
PCOS is diagnosed in women having at least 2 of these 3 symptoms:
- Irregular menstrual cycles
- Elevated androgen levels
- Cysts in the ovaries

A careful history and exam will reveal most, if not all of the above.
Women with PCOS will typically present with a history of irregular periods, skipping months at a time, and/or prolonged and heavy menstrual cycles.
A lot of women will note increased facial hair, increased hair on the lower abdomen, etc. This is usually visible on exams and is a sign of increased androgen levels. Increased acne is also a sign of high androgen levels.
An ultrasound will diagnose cysts on ovaries. PCOS ovaries are characterized by increased follicles, oft times described as a string of pearls appearance due to the way the follicles surround the periphery of the ovary.
When patients or consulting physicians ask for “blood work” to evaluate PCOS; things that are commonly ordered include:
- Cholesterol levels (HDL, LDL, Triglycerides)
- Androgen levels (DHEAS, Total and Free Testosterone)
- Fasting Insulin
- Screening for diabetes with a 2-hour glucose tolerance test
Pregnancy and PCOS
With irregular cycles, one can imagine the impact of PCOS on fertility. 80% of women with PCOS have fertility issues. Anovulation (lack of ovulation) being the primary cause.
Women with PCOS oftentimes will seek the help of a specialist, an REI (reproductive endocrinology and infertility), to achieve pregnancy. Through the use of fertility treatments aimed at improving ovulation, women with PCOS are able to conceive.
While PCOS can certainly make getting pregnant challenging, even once pregnancy is attained, there are still risks. These will likely include:
- Preterm delivery,
- Hypertensive disorders of pregnancy, like preeclampsia
- Gestational diabetes
Managing PCOS Through Diet and Exercise

Lifestyle modification pays dividends. I tell my patients this all the time.
Eating healthy and staying active certainly decreases the risk of developing certain diseases like high cholesterol, diabetes, and high blood pressure.
In many instances, diet and exercise can treat or improve these ailments that may already exist in some individuals.
PCOS is no different. With as little as 5-10% body weight loss, menstrual cycle regulation, PCOS symptoms can be improved. Weight loss improves cholesterol levels, decreases insulin, and decreases the risk for diabetes and heart disease.
In studies analyzing diets for treating PCOS, low carbohydrate diets were found to be effective for both weight loss and lowering insulin levels. Diets with a low glycemic index were found to be superior to regular weight loss diets for regulating menstrual cycles.
Studies support that 30 minutes of moderate-intensity exercise three times per week can help women with PCOS effectively lose weight. Weight loss via exercise improves ovulation and insulin levels.
Diet and exercise are synergistic because they are more effective in helping to achieve weight loss together, as opposed to doing one without the other.
Common Medical Treatment for Polycystic Ovary Syndrome (PCOS)
Birth control pills are a common option. They help regulate menstrual cycles, are protective against endometrial cancer, and help decrease androgen levels which in turn will treat things like acne, and increased hair growth.
Metformin is an insulin sensitizer and helps improve insulin levels in women affected with PCOS. When used in conjunction with diet and exercise, it has been found to improve weight loss, decrease blood sugar levels, as well as improve menstrual cycles.
Clomid. Clomiphene citrate, aka, Clomid, is a fertility medication commonly used to treat ovulatory dysfunction. Twins and other multiple births have been associated with Clomid.
PCOS and excess hair. While birth control pills help lower androgen levels, and thus, decrease hair growth, other options for treating unwanted hair commonly associated with PCOS include laser treatment and electrolysis. Vaniqa (Eflornithine), is a prescription cream that helps slow hair growth.
Conclusion
Although PCOS encompasses a lot, it is manageable.
I hope this blog post has made this common ailment easier to understand, and provided you with adequate information to help you or someone you know as they deal with PCOS.
Got questions? Leave them in the comments, I will be happy to answer them. Don’t forget to share this post with someone that will find it helpful.
Until next time,
Choose Happiness.
Dr. Angela.